Executive Summary:
| Older adults and people with disabilities cannot equitably access the same health information and care as people without disabilities when hospital websites are not accessible. As stated in the American Health Information Management Association (AHIMA) policy statement on individual access to care, challenges such as these must be addressed, especially as more people rely on technology to interact with the health care system. | |
|
This issue brief: |
|
|
|
|
|
|
|
Background:
During the pandemic, Kaiser Health News found that websites providing registration for and information on COVID-19 vaccination violated disability rights laws, hindering the ability of vulnerable populations to sign up for and receive the potentially life-saving vaccine. For people with disabilities, this occurrence is all too common. Currently, the most prevalent Americans with Disabilities Act (ADA) lawsuit in the health care setting is not about physical access to a location but about the lack of accessible and effective communication.
Web Accessibility and Population Health
Web accessibility, or digital accessibility more broadly, involves designing content to be inclusive of people who have visual, motor, auditory, speech, or cognitive disabilities. More than 61 million people in the United States (nearly 1 in 4) and over 1 billion people worldwide have one of these disabilities, including 46 percent of people ages 60 and older.
The World Wide Web Consortium (W3C), the primary international standards organization for the internet, researched the needs of older web users to develop guidance on accessibility. W3C’s review of disability-related statistics revealed that:
- 47 percent of people ages 61 to 80 have some hearing loss
- 16 percent of people ages 65 to 74 have significant vision loss that can’t be corrected
- At least 50 percent of people over age 65 have arthritis or other conditions affecting motor skills
- Around 20 percent of people ages 70 or older have mild cognitive impairment, which might include short-term memory limitations, difficulty with concentration, or other symptoms
The researchers concluded that the W3C’s Web Content Accessibility Guidelines (WCAGs) address most of these needs. Websites that meet the Level AA success criteria in the latest version of the WCAGs are reasonably accessible for most people with disabilities, including adults who have changing abilities due to aging, and often improve usability for everyone in general.
The WCAG includes the following four principles:
- Perceivable. Information and user interface components must be presentable to users in ways they can perceive.
- Operable. User interface components and navigation must be operable.
- Understandable. Information and the operation of the user interface must be understandable.
- Robust. Content must be robust enough that it can be interpreted reliably by a wide variety of user agents, including assistive technology.
These guidelines are currently on iteration 2.1 and are referred to as WCAG 2.1.
Health Literacy for Health EquityTM
In October 2021, as part of the Health Literacy for Health Equity initiative, AHIMA Foundation conducted a nationwide survey on how Americans access and use their health information. A key finding of the survey is that medical records are a vital part of health management, but millions of Americans have difficulty accessing their information.
To “increase the proportion of people who can view, download, and send their electronic health information,” as described in one of the HealthyPeople 2030 objectives developed by the Health Communication and Health Information Technology Workgroup, we first need to address the barriers to digital access for the most vulnerable members of the population.
Historically, the focus of hospitals and healthcare systems has been on caring for patients and saving lives—the social pillars of environmental, social, and corporate governance. But these hospitals and systems could benefit from embedding more social impact into their overall strategy.
An August 2021 report from PricewaterhouseCoopers’s Health Research Institute showed that many health care organizations have internal initiatives underway to enhance diversity and inclusion programs and increase staff skills. For example, Mass General Brigham launched new programs in 2021 to provide patients access to physical devices like tablet computers, software technologies like web access and digital tools, and digital literacy training.
![]()
“Most websites and electronic medical record systems are not made in such a way that they're compatible with assistive technology. For me, this means that I cannot use a screen reader on my phone or computer to send messages to healthcare providers, review test results, interpret and pay medical bills or refill medications.”
– Corbb O’Connor, age 34, Minneapolis, Minnesota, living with a disability
The American Hospital Association’s (AHA’s) Health Equity Roadmap, launched in 2022, provides a framework to help hospitals and health care systems throughout the U.S. chart their own paths toward becoming more equitable and inclusive. Notably and of importance to the topic of web accessibility, the roadmap includes creating an infrastructure to maintain accountability for sustaining diversity, equity, and inclusion work across departments and service lines and investing in strong hospital-community partnerships.
| Hospitals and health care systems in the U.S. need continuing education on the role of web accessibility in ADA compliance given the significance of newly issued federal guidance. |
![]()
“The pandemic really opened our eyes to meeting community members where they were – often at home. We implemented telehealth as federal and state regulatory waivers allowed, including reproductive health and mental health services. As this new method of service delivery rolled out, my colleagues and I questioned the literacy level of the forms, instructions, and services we provided. COVID-19, for all intents and purposes, helped us begin seeing things from the perspective of our patients in a better and more equitable light. Outside of a public health emergency, digital accessibility is something we should care about or take ownership of as health information professionals.”
– Aurae Beidler, MHA, RHIA, CHC, CHPS, Director-elect to the AHIMA Board of Directors & Former Compliance and Privacy Officer at the Linn County Department of Health Services in Albany, Oregon
Federal Requirements for Providing Accessible Care
Several federal laws, including the Rehabilitation Act of 1973, the ADA of 1990, and the Affordable Care Act of 2011, require health care organizations to provide patients who have disabilities with equitable health care through the provision of accommodations. And in 2017, Section 508 of the ADA was updated to include WCAG standards in response to market trends and innovations in technology.
Recent Federal Guidance for Web Accessibility and Nondiscrimination in Telehealth
On March 18, 2022, the U.S. Department of Justice’s (DOJ’s) Civil Rights Division issued Guidance on Web Accessibility and the ADA, explaining how state and local governments (entities covered by ADA Title II) and businesses open to the public (entities covered by ADA Title III) can ensure their websites are accessible to people with disabilities, in line with the ADA’s requirements. On July 29, 2022, the U.S. Department of Health and Human Services Office of Civil Rights issued Guidance on Nondiscrimination in Telehealth, providing clarity on how federal nondiscrimination laws require accessibility for people with disabilities and limited English proficiency in any care provided via telehealth.
DOJ makes it clear that businesses, including hospitals and medical offices, must ensure that the programs, services, and goods they provide to the public—including those provided online—are accessible to people with disabilities.
![]()
"Telehealth has the potential to decrease healthcare disparities for patients with disabilities as it reduces transportation barriers, but it can also increase disparities if it is not accessible to those who have hearing, cognitive, vision, or other communication disabilities. Evidence is needed to inform both the development and implementation of accessible telehealth and other healthcare."
– Disability Equity Collaborative
| The home pages of most top U.S. hospitals have many accessibility errors and are not compliant with WCAG 2.1 criteria. |
Baseline Data Findings
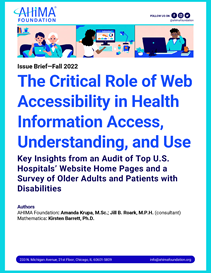
In August 2022, AHIMA Foundation and Mathematica worked together to gather and analyze baseline data on the state of accessibility compliance across the website home pages of top U.S. hospitals. We gathered these data using web accessibility evaluation tools—software programs or online services that help determine if web content meets accessibility guidelines.
We used the 2021–2022 U.S. News & World Report’s annual rankings of best hospitals to identify the ”honor roll” hospitals and the top hospitals in each of the following specialties: rehabilitation, geriatrics, diabetes and endocrinology, cancer, and cardiology and heart surgery. Across the honor roll and specialty lists, 106 unique hospitals were represented. We selected their home pages for analysis because those pages represent the “digital front door” of the hospital.
Using accessScan, a free online evaluation tool designed to give an overall compliance score for a web page to raise awareness about the need for accessibility, we gathered and analyzed data on each of the hospitals’ home pages.
We found that only 4.9 percent of hospitals on the honor roll or the top hospital lists were WCAG 2.1 compliant. Nearly 80 percent of the hospitals were semicompliant, and 16.7 percent were noncompliant. Rehabilitation hospitals had the most hospitals deemed compliant, at 12.2 percent, and geriatrics hospitals had the fewest, at 4.3 percent (Figure 1).
Limitations of Automated Accessibility Testing Tools
According to W3C, all accessibility aspects cannot be checked automatically; human judgment is required. But accessibility evaluation tools such as accessScan can help you quickly identify potential accessibility issues and give you a starting place for a manual review. WAVE is another great example of an automated (AI-based) accessibility testing tool designed to support manual evaluation and help you better understand accessibility issues. Similarly, Google Lighthouse offers a clear gauge of digital accessibility, providing a score that you can track and measure against as you make improvements.
Accessibility testing tools don’t guarantee compliance. Although the term “semicompliant” gives the impression that a website might need only a few fixes to be compliant, for patients with disabilities, a semicompliant site is one that they will likely have trouble navigating.
| Older adults and patients with disabilities face barriers to accessing their health information electronically; many have struggled to use a hospital website or patient portal. |
Patient-Centered Outcomes Research
To document and understand patients’ experiences when accessing their health information electronically, AHIMA Foundation conducted a qualitative survey of older adults and people with disabilities in August 2022 with Knowbility, a nonprofit organization whose mission is to create an inclusive digital world for people with disabilities.
Participants included people who have low vision, have mobility-related disabilities, are Deaf or hard of hearing, or have a cognitive disability. Other organizations, including the Christopher & Dana Reeve Foundation, the National Digital Inclusion Alliance, the Disability Equity Collaborative, and the Digitunity, also promoted the survey through their networks to increase the sample size and obtain additional perspectives from people with disabilities and older adults.
The survey responses highlight the issues that people with disabilities face on a daily basis when trying to access information digitally. Accessibility errors on websites include poor color contrast; the use of color alone to convey information; a lack of text alternatives (or “alt text”) on images, required by screen readers; videos with no captioning; online forms that are not accessible to screen readers; and navigation that requires a mouse. When asked whether living with a disability affects their ability to access information on the internet, participants gave specific examples of limited accessibility.
| Source: Improving Access to Electronic Health Information for Older Adults and People with Disabilities, AHIMA Foundation, 2022 | |
|
Q: Does living with a disability impact your ability to access information on the internet? |
|
 |
R1: Yes. Mostly I use the internet visually with browser zoom and high contrast mode or browser color changing, but I also use screen reading software. Both of these things (and at times both at once) can have problems with websites, making their content out of my reach. |
|
R2: Yes. I do not have access to podcasts. Many videos are not captioned or not captioned correctly. What would make it easier is requiring all videos and streaming content to be captioned and therefore accessible. |
|
|
R3: Yes. Many sites and applications are still not properly keyboard accessible. Having the ability to navigate throughout a website with only my keyboard would be hugely beneficial. |
|
|
R4: Yes. Being able to understand and find information can be challenging. It can get very distracting. I just don't have the patience. |
|
As health care websites, patient portals, and health-related apps become more advanced and intricate, accessibility declines. Health literacy extends beyond being able to read and understand health content online; it also includes the ability to access and use personal health information.
When asked whether it is easy to access their health information electronically, such as blood-test results or after-visit summaries, patients described healthcare-specific accessibility issues, and many shared the need for someone to assist them. Needing someone to help access private and protected health information is a threat to both patient privacy and personal dignity. Although patient privacy is protected by the well-known Health Insurance Portability and Accountability Act of 1996 (HIPAA), dignity is a human right that is not federally protected. Yet human dignity is the founding moral principle of a human rights framework that is truly inclusive and universal while recognizing the particular needs and living conditions of people with diverse impairments. Violations of someone’s dignity indicate a systematic disregard of their human rights.
When asked to describe a time when they struggled to use a hospital or health care website, access their health information, or make a doctor’s appointment, patients shared experiences of frustration, along with recommendations for making health information more accessible.
|
Q: Is it easy for you to access your health information electronically, for example, blood test results or after-visit summaries? |
|
| Source: Improving Access to Electronic Health Information for Older Adults and People with Disabilities, AHIMA Foundation, 2022 | |
 |
R1: No. The data is often presented as charts or tables that aren't readable with a screen reader. Additionally, many times the data are only available as untagged PDFs, which means that I cannot easily move around the document except read it from start to finish. |
|
R2: I have someone help me. Certain fonts are difficult to read. |
|
|
R3: Yes. Only if it is e-mail or online sign-in access. If it's by phone, this makes it harder. |
|
|
R4:I have someone help me. Test results are too hard to find on a page, online or otherwise. I can usually remember those numbers when they're given to me verbally. If it's something like a treatment plan, or messages online from healthcare providers and I’m just seeking a tiny piece of info, it's simply too hard to find in most cases. |
|
| Source: Improving Access to Electronic Health Information for Older Adults and People with Disabilities, AHIMA Foundation, 2022 | |
|
Q: Tell us about a time where you struggled to use a hospital or healthcare website, access your health information, or set up a doctor’s appointment. |
|
 |
R1: I tried to go onto my health system's website, but I was unable to adjust the font big enough so I could see it. My magnifying glass was inadequate. It would have helped to have a digital magnifier on the website to enlarge font. |
|
R2: When I was changing health insurance, I had to pay a bill on the hospital's website and couldn't figure out how to do that. The tab that I needed was not easily accessible with a keyboard. |
|
|
R3: When my baby was born I was not able to access anything including my discharge paperwork and prescriptions on the hospital patient portal. All the documents and hospital records were provided to me in print, and I cannot see to access them. It would have been nice to have access to MyChart and provide me everything in Braille. |
|
|
R4: I often call to make appointments because I don't want to struggle with the website. However, when the telephone hold time exceeded one hour, I went to the online patient portal and struggled to navigate to the right part of the portal, had trouble finding my provider in the list of options, then found that the date picker was only functional with a mouse. |
|
The survey responses showed that there are some success stories in web and digital accessibility. When asked to describe a time when it was easy to access a hospital or health care website, access health information, or make a doctor’s appointment, participants described sites that they could easily navigate, the ability to access information by themselves and the ways in which having their personal health information improved their care.
|
Q: Tell us about a time when it was easy to access a hospital or health care website, access your health information, or set up a doctor’s appointment. What made it easy for you? |
|
| Source: Improving Access to Electronic Health Information for Older Adults and People with Disabilities, AHIMA Foundation, 2022 | |
 |
R1: I like the VA Healthcare website which syncs up well with my assistive software. There are very few problems on that one because of the compatibility. |
|
R2: About 3 or 4 months ago on the Aurora Healthcare MyChart site I was able to find the results of my COVID-19 test. What made it easy was that it was in an area on the site that was in the right spot and worded correctly to grab my attention. |
|
|
R3: I went on to the Mayo Clinic website and the presentation with font size was the right fit to accommodate my disability. Combined with my magnifying glass, I was self-reliant. |
|
|
R4: When reading my test results with one provider, the result page clearly indicated the name of each test, my result, and the normal range. I was able to easily peruse these results while waiting for the doctor to come into the room, and we had a deeper discussion as a result. |
|
|
Multisectoral collaboration, including user-based testing with patients with disabilities and older adults, is needed to improve digital accessibility in the healthcare ecosystem. |
An accessibility audit is only the first step. Accessibility audit tools inspect a web page for accessibility problems and produce a list of potential errors they deem worth human investigation. But audit tools should be used only to highlight the need for website remediation. Website compliance testing with actual patients is a necessary next step, as accessibility is about the patient experience.
![]()
“Web inaccessibility prevents those that often need life-changing, life-saving healthcare from accessing it online wherever they live. The Digital Equity Act programs will empower Americans with disabilities to independently navigate digital healthcare systems and utilize websites that are designed to respond to their needs.”
– Angela Thi Bennett, Director of Digital Equity, National Telecommunications and Information Administration, U.S. Department of Commerce
Beware of the quick fix. Despite recent advances in technology, well-intentioned website accessibility overlay tools powered by artificial intelligence (AI) sometimes make accessibility issues even worse for people with disabilities, according to a July 2022 investigation by The New York Times. In 2021, over 700 accessibility advocates and web developers signed an open letter calling on organizations to stop using these tools, writing that the practical value of the new features was “largely overstated” and that the “overlays themselves may have accessibility problems.”
Collaboration is key. Collaborating within the hospital across administration, management, and operations will help ensure that you can effectively work together to correct errors and improve accessibility. For example, color contrast and other color errors on the hospital home page might be an issue that falls under the hospital’s brand guidelines and within the purview of marketing. Working with groups outside of your institution such as community advocacy groups, local centers for independent living, and ADA regional centers will ensure that you are engaging the disability community in the development of solutions.
Hire and train digital accessibility experts. For long-term compliance, accessibility experts suggest that organizations hire and train full-time employees to oversee digital accessibility efforts, rather than contracting out remediation work for a one-time website overhaul. Experts highly recommend naming a “digital accessibility coordinator” and setting up a work group that includes decision makers from information technology; health information management; human resources; diversity, equity, and inclusion; procurement/vendor selection; and marketing and brand management departments.
|
Case Study: Perkins Access & Spaulding Rehabilitation Hospital Perkins Access is a consultancy group within the world-renowned Perkins School for the Blind, helping organizations build accessible digital experiences for their clients, in this case, the patients of Spaulding Rehabilitation Hospital. This case study offers a unique look at the accessibility remediation of a leading hospital website with an end-user focus -- creating an inclusive patient experience at their digital front door. |
![]()
“Accessibility is the law. It’s also a gateway to a community of millions of Americans who have disabilities that affect how they use the web, enabling healthcare organizations to reach and serve more potential patients. So there are clear business reasons for embracing digital accessibility. Most importantly, it’s just the right thing to do.”
– Luiza Aguiar, Executive Director, Perkins Access
Conclusion:
Currently, the U.S. health care system is failing its patients with disabilities and older adults on the digital front. Most top hospitals in the country are not compliant with WCAG 2.1 standards for digital accessibility. No health care facility in the nation would leave its main entrance inaccessible to patients with disabilities, and yet those same patients might not be able to enter the facility’s digital front door. Websites and digital tools such as apps that have been thoughtfully designed or remediated for people with a broad range of impairments, injuries, and disabilities will benefit everyone and improve the patient experience for all. It is imperative that all health care organizations consider the broad diversity of users’ functional needs when developing and maintaining digital media.
References:
-
accessiBe. “Find Out If Your Website Is ADA & WCAG Compliant.” n.d. https://accessibe.com/accessscan.
-
AHA Institute for Diversity and Health Equity. “Community Collaboration for Solutions.” n.d. https://equity.aha.org/levers/community-collaboration-solutions.
-
AHA Institute for Diversity and Health Equity. “Systemic and Shared Accountability.” n.d. https://equity.aha.org/levers/systemic-and-shared-accountability.
-
AHA Institute for Diversity and Health Equity. “The Health Equity Roadmap.” n.d. https://equity.aha.org/.
-
AHIMA Foundation. “Understanding, Access, and Use of Health Information in America.” October 2021.
-
AHIMA. “Individual Access to Health Information: Advocacy.” n.d. https://www.ahima.org/advocacy/policy-statements/individual-access-to-health-information/.
-
Assistant Secretary for Public Affairs. “About the ACA.” HHS.gov, March 15, 2022. https://www.hhs.gov/healthcare/about-the-aca/index.html.
-
Centers for Disease Control and Prevention. “Disability Impacts All of Us.” Infographic. September 16, 2020. https://www.cdc.gov/ncbddd/disabilityandhealth/infographic-disability-impacts-all.html.
-
Christopher & Dana Reeve Foundation. Home page. n.d. https://www.christopherreeve.org/.
-
Digitunity. “About Us.” August 17, 2021. https://digitunity.org/about-us/.
-
Disability Equity Collaborative. “Patient-Centered Outcomes Research Priorities to Advance Disability Equity.” 2021. https://www.disabilityequitycollaborative.org/wp-content/uploads/2021/08/2021-DEC-Whitepaper.pdf.
-
DOJ, Civil Rights Division. “ADA Requirements: Effective Communication.” January 2014. https://www.ada.gov/effective-comm.htm.
-
DOJ, Civil Rights Division. “Americans with Disabilities Act of 1990, as Amended.” Updated June 15, 2009. http://www.ada.gov/pubs/adastatute08.htm.
-
DOJ, Civil Rights Division. “Barrier-Free Health Care Initiative.” n.d. https://www.ada.gov/usao-agreements.htm.
-
DOJ, Civil Rights Division. “Guidance on Web Accessibility and the ADA.” March 18, 2022. https://beta.ada.gov/resources/web-guidance/.
-
Graumann, Sigrid. “Human Dignity and People with Disabilities.” In The Cambridge Handbook of Human Dignity, edited by Marcus Düwell, Jens Braarvig, Roger Brownsword, and Dietmar Mieth. Cambridge University Press, 2015. https://www.cambridge.org/core/books/abs/cambridge-handbook-of-human-dignity/human-dignity-and-people-with-disabilities/589EDD2CE3E2223046556C63ACC8DAB4.
-
Knowbility. “Digital Accessibility Advocacy, Training, and Consulting.” n.d. https://knowbility.org/.
-
Mass General Brigham. “Mass General Brigham Launches New Digital Health Initiatives.” July 15, 2021. https://www.massgeneralbrigham.org/en/about/newsroom/press-releases/mass-general-brigham-launches-new-digital-health-initiatives.
-
Morris, Amanda. “For Blind Internet Users, the Fix Can Be Worse Than the Flaws.” The New York Times, July 13, 2022. https://www.nytimes.com/2022/07/13/technology/ai-web-accessibility.html.
-
National Telecommunications and Information Administration. “Digital Equity Act Programs.” n.d. https://www.internetforall.gov/program/digital-equity-act-programs.
-
Office of Disease Prevention and Health Promotion, U.S. Department of Health and Human Services. “Increase the Proportion of People Who Can View, Download, and Send Their Electronic Health Information—HC/Hit‑d09.” n.d. https://health.gov/healthypeople/objectives-and-data/browse-objectives/health-it/increase-proportion-people-who-can-view-download-and-send-their-electronic-health-information-hchit-d09.
-
Overlayfactsheet.com. “Overlay Fact Sheet.” n.d. https://overlayfactsheet.com/.
-
Perkins School for the Blind. “Perkins Access and Spaulding Rehab Open New Digital Door to Patients with Disabilities.” October 25, 2021. https://www.perkins.org/perkins-access-and-spaulding-rehab-open-new-digital-door-to-patients-with-disabilities/.
-
PricewaterhouseCoopers. “Health Industries.” n.d. https://www.pwc.com/us/en/industries/health-industries.html.
-
Scorse, Yvette, Vicky Yuki, and Lo Smith. “Home.” National Digital Inclusion Alliance, n.d. https://www.digitalinclusion.org/.
-
Section508.gov. “IT Accessibility Laws and Policies.” n.d. https://www.section508.gov/manage/laws-and-policies/.
-
U.S. Department of Health and Human Services and DOJ. “Guidance on Nondiscrimination in Telehealth: Federal Protections to Ensure Accessibility to People with Disabilities and Limited English Proficient Persons.” https://www.hhs.gov/sites/default/files/guidance-on-nondiscrimination-in-telehealth.pdf.
-
U.S. Equal Employment Opportunity Commission. “The Rehabilitation Act of 1973.” n.d. https://www.eeoc.gov/statutes/rehabilitation-act-1973.
-
U.S. News & World Report. “America’s Best Hospitals: The 2022–2023 Honor Roll and Overview.” July 26, 2022. https://health.usnews.com/health-care/best-hospitals/articles/best-hospitals-honor-roll-and-overview.
-
U.S. News & World Report. “Best Hospitals for Cancer.” n.d. https://health.usnews.com/best-hospitals/rankings/cancer.
-
U.S. News & World Report. “Best Hospitals for Cardiology & Heart Surgery.” n.d. https://health.usnews.com/best-hospitals/rankings/cardiology-and-heart-surgery.
-
U.S. News & World Report. “Best Hospitals for Diabetes & Endocrinology.” n.d. https://health.usnews.com/best-hospitals/rankings/diabetes-and-endocrinology.
-
U.S. News & World Report. “Best Hospitals for Geriatrics.” n.d. https://health.usnews.com/best-hospitals/rankings/geriatric-care.
-
U.S. News & World Report. “Best Hospitals for Rehabilitation.” n.d. https://health.usnews.com/best-hospitals/rankings/rehabilitation.
-
United Nations. “United Nations Enable | Disability.” n.d. https://www.un.org/development/desa/disabilities/.
-
W3C, WAI. “Selecting Web Accessibility Evaluation Tools.” Updated December 23, 2017. https://www.w3.org/WAI/test-evaluate/tools/selecting/.
-
W3C, Web Accessibility Initiative (WAI). “Older Users and Web Accessibility: Meeting the Needs of Ageing Web Users.” Updated August 14, 2020. https://www.w3.org/WAI/older-users/.
-
W3C. “Web Accessibility Evaluation Tools List.” Updated March 2016. https://www.w3.org/WAI/ER/tools/.
-
W3C. “Web Content Accessibility Guidelines (WCAG) 2.1.” June 2018. https://www.w3.org/TR/WCAG21/.
-
WebAIM. “Wave Web Accessibility Evaluation Tool.” n.d. https://wave.webaim.org/.
-
Weber, Lauren, and Hannah Recht. “COVID Vaccine Websites Violate Disability Laws, Create Inequity for the Blind.” Kaiser Health News, January 7, 2022. https://khn.org/news/article/covid-vaccine-websites-violate-disability-laws-create-inequity-for-the-blind/.
|
Suggested Citation: Krupa, A., J.B. Roark, and K.B. Barrett. “The Critical Role of Web Accessibility in Health Information Access, Understanding, and Use" (Issue brief). Chicago, IL: AHIMA Foundation, 2022. |